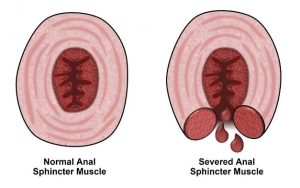
The anal sphincters constitute a set of 2 muscles that form a ring around the anus and are crucial in maintaining continence mechanism in the body. The anal sphincter is a complex muscular structure that comprises two main components: the inner, involuntary (smooth) muscle called the internal anal sphincter and the outer, voluntary (striated) muscle known as the external anal sphincterInternal Anal Sphincter: The internal anal sphincter is an involuntary muscle that remains contracted at rest. It serves as the primary barrier to prevent involuntary bowel movements. It’s crucial in maintaining continence by preventing fecal matter from escaping the rectum.
External Anal Sphincter: The external anal sphincter is a voluntary muscle that we can consciously control. It plays a secondary role in maintaining continence and allows us to voluntarily open the anus for defecation.
While the anal sphincter is a workhorse, injury or damage to the muscles can have significant consequences, such as:
- Fecal incontinence or leakage
- Pain
- Bleeding
- Perineal cellulitis
- Enteric fistulae
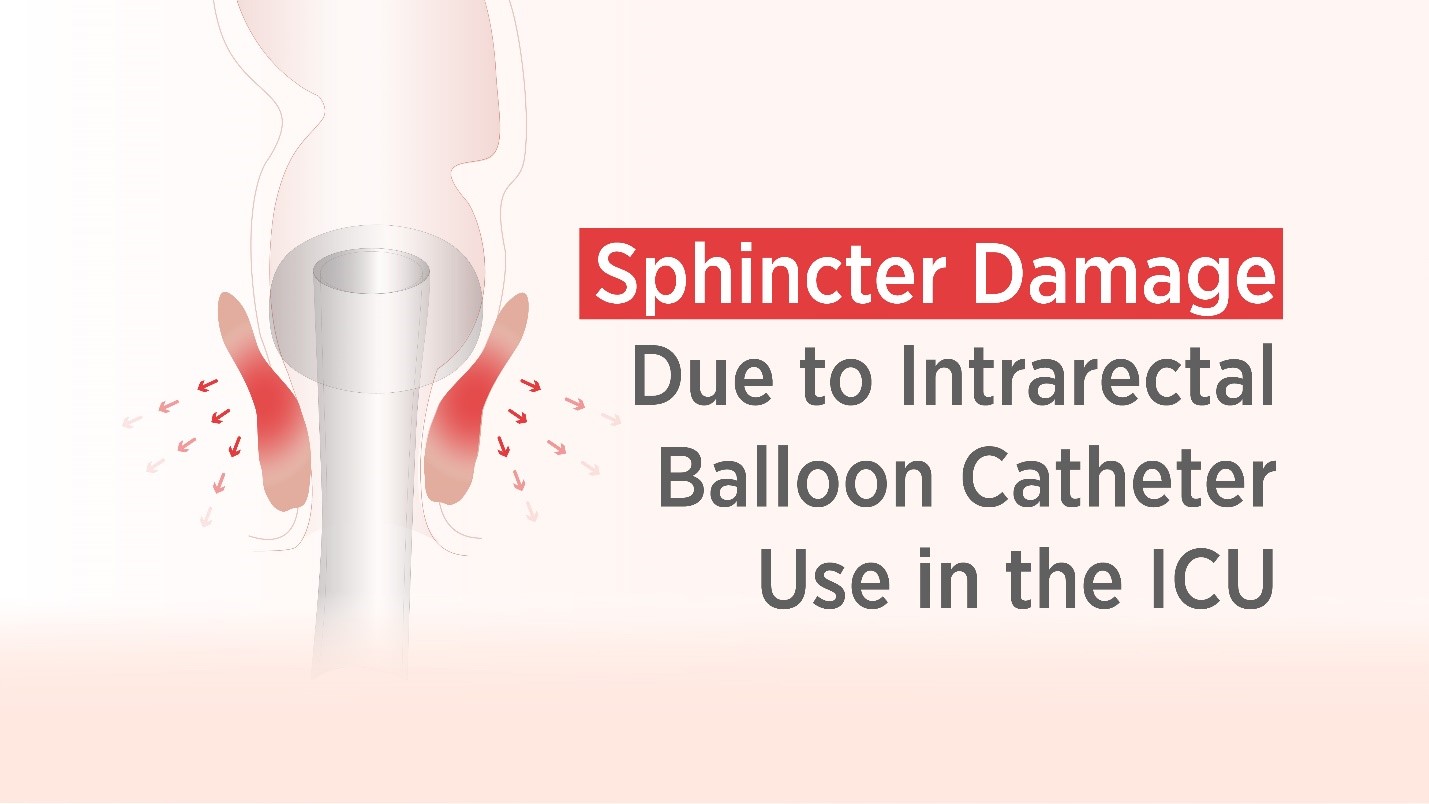
ICU nurses frequently use intrarectal balloon catheters (IBCs) to manage fecal incontinent patients, but these devices can damage anal sphincter muscles. Since balloon catheters rely on inflating the balloon and a tonic sphincter, in some cases, nurses observe fecal leakage and spontaneous expulsions. To keep IBCs in place and to prevent potential leakage, users often fill the retention balloon with more liquid or air than recommended by the manufacturer. The practice is surprisingly common – in a recent study of 50 patients who had an IBC, over-inflation was the most common problem, with 14 percent of participants having an over-inflated retention balloon.
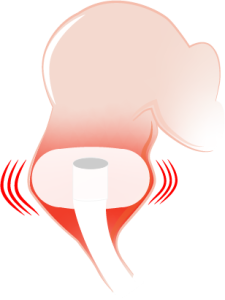
Prolonged pressure on the rectal mucosa can cause tissue damage, leading to inflammation, irritation, and ulceration. In severe cases, excessive pressure from the balloon can cause tissue necrosis (cell death), often requiring additional medication, and even surgical intervention.
Each of these can cause systemic issues that can compromise patient health, extend stays, and even worsen fecal incontinence – sphincter damage from these complications can also increase the patient’s susceptibility to hospital-acquired infections (HAIs), also known as healthcare-associated infections.
Inappropriate use, improper insertion, overinflation of balloon catheters and leaving an IBC in too long can increase the risk for these complications.
Qoramatic Soft Receptacle exerts 0 mmHg radial pressure

Leakage is a common concern with intrarectal balloon catheters, but Qoramatic is designed to minimize the risk of leakage, reducing the chances of skin breakdown, pressure ulcers, and related hospital acquired infections. Efficient proactive fecal diversion helps reduce complications and discomfort, enhancing overall nursing satisfaction and superior clinical outcomes for patients.