Managing fecal incontinence is challenging for patients in the intensive care unit (ICU) and the healthcare staff who care for them.
Traditional fecal management solutions involve the use of absorbent pads and intrarectal balloon catheters. While these methods help to manage fecal effluents, these are associated with various clinical complications.
ICU Patients are at Special Risk of Complications associated with Fecal Incontinence
Up to a forty percent of all intensive care patients experience fecal incontinence. The critical nature of ICU often requires patients to undergo a range of invasive medical procedures, prolonged immobilization, and medication regimens that can disrupt their gastrointestinal function. Prolonged bed rest, coupled with the side effects of medications and the stress of their critical condition, can weaken the muscles responsible for bowel control. In the already challenging environment of intensive care, addressing fecal incontinence is crucial not only for the comfort and dignity of patients but also to reduce the risk of serious and potentially life-threatening infections associated with this condition.
Fecal incontinent patients have a higher risk for skin irritation and breakdown from prolonged or repeated exposure to stool, and are more susceptible to the infectious pathogens in feces. Research shows that the use of sedative drugs, coma status, greater bowel movement frequency, higher Perineal Assessment Tool (PAT) scores, and loose stool are independent risk factors for IAD among ICU patients with fecal incontinence.
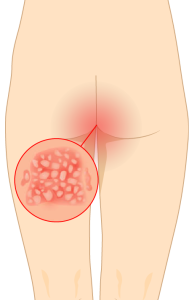
Adequate fecal effluent management is required to reduce constant skin exposure to fecal effluents, and to decrease complications and costs .
Comparing Three Fecal Management Systems
Absorbent pads
Absorbent pads are the least efficient fecal management solution in that they protect the bed but not the patient. Skin is directly exposed to fecal exudate. In fact, absorbent pads can hold the feces against the patient’s skin until the next bed check and change, and this can be hours after the patient had a bowel movement. Absorbent pads also require turning and repositioning the patient frequently to change the pads, linen and clean the patients. These activities are time consuming and labor intensive which can lead to increase on nursing time, nurse exhaustion and fatigue. Also absorbent pads are open system which can easily facilitate cross contamination and lead to various hospital acquired infections such as c.difficile.
Balloon catheters
Balloon catheters are more efficient than absorbent pads in preventing feces from coming in contact with the skin. In these systems, stool passes through a lumen in a catheter tube into a collection bag; a balloon holds the device in place inside the patient’s rectum. While these systems work well in theory, they may not function as well in practice.
Overinflation to control leakage is a huge, yet under-acknowledged and under-reported problem. In one study, 14 percent of patients with complications experienced over-inflation, 8 percent had poor anal sphincter tone leading to tube expulsion, and another 4 percent had excessive leakage of fecal effluent around the device.
Introducing Qoramatic – the Innovative Solution for Efficient Fecal Management

Unlike other fecal management systems that passively rely on peristalsis, Qoramatic is an industry first automated fecal management system that employs negative pressure suction to proactively divert fecal effluents. The device employs a soft teat/receptacle that exerts 0 mmHg radial pressure on the rectal mucosa minimizing any risk of rectal trauma, mucosal impairment, and injury. No inflation or over inflation eliminates challenges and medical errors associated with high pressure balloons.
Leakage is a common concern with intrarectal balloon catheters, but Qoramatic is designed to minimize the risk of leakage, reducing the chances of skin breakdown, pressure ulcers, and related hospital acquired infections. Efficient proactive fecal diversion helps reduce complications and discomfort, enhancing overall nursing satisfaction and superior clinical outcomes for patients.
For more information on Qoramatic, contact Consure Medical today.

