Urinary incontinence is a concerning issue, affecting more than 50% of postmenopausal women. This condition usually occurs in 20-30% of young women, about 30-40% in middle age and 50% in old age women. For most women, the onset of menopause initiates a way for a whole host of symptoms such as night sweats, moodiness, hot flashes and many more. But there is one common symptom which is sometimes unrecognized – loss of bladder control also referred to as urinary incontinence. The involuntary loss of control could be minor, cause accidental leakage and can be experienced while coughing, laughing or sneezing.
Why does menopause cause loss of bladder control
Before the onset of menopause several unpleasant symptoms worsen the quality of life for a woman. The symptoms are a result of different hormonal and metabolic changes which can increases the chances of chronic diseases. The ovaries of women stop making estrogen hormone as they are near the menopause period. The hormone is responsible for keeping bladder and urethra healthy, and reduced level of estrogen can weaken the pelvic muscles. These muscles help to prevent sudden loss of urine and fecal effluents. The decreasing level of hormone can initiate the onset and worsen urinary incontinence.
Furthermore, with increasing age of women, their bladders lose elasticity. When the bladder fills up with urine, the lack of elasticity can decrease the ability to stretch and retain urine, and hence causes an overactive bladder. An overactive bladder can cause to urine flow more frequently. The lack of estrogen can cause dryness of the anatomy which can increase risk of urinary tract infections and accounts in over 50% of menopausal women. It is necessary to follow a treatment for urinary tract infection and CAUTI Prevention strategies because the infection can spread to other parts of the body and cause serious health problem.
Bladder issues faced by post-menopausal women
Stress incontinence – It occurs when tissue supporting urethra becomes weak. Individuals experience stress incontinence while doing several physical activities such as lifting heavy items or doing something which puts pressure on the bladder.
Urge incontinence – Urge Urinary incontinence causes an involuntary and urgent need to urinate several times in day and night. It is caused by abnormal contractions in the bladder. Usually, sphincter muscles control the urine flow from the bladder but with urge incontinent patients the muscles of the bladder are contracted with enough force to override sphincter muscles of urethra and can cause involuntary leakage.
Painful Urination – After menopause, women are more likely to experience urinary tract infections or burning sensation while urinating. Some women also suffer through pain and irritation more frequently than usual. These symptoms of genital and urinary tract are together known as genitourinary syndrome of menopause.
Bladder issues faced by post-menopausal women
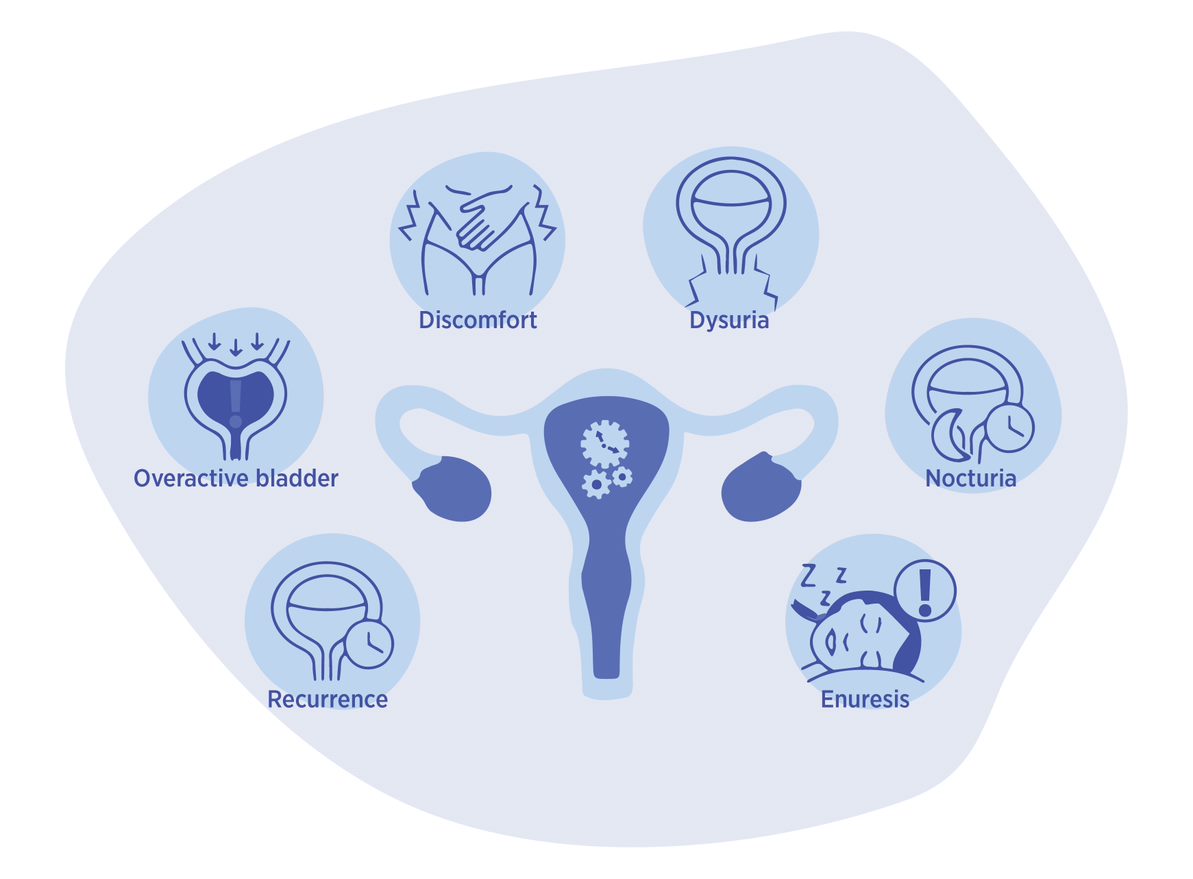
Symptoms of Urinary incontinence during menopause
Involuntary bladder control is a common problem in menopause women. They experience many symptoms other than leakage. It is necessary to monitor these symptoms which are affecting the body to improve the quality of life. Some symptoms include: –
- Recurrence – frequency of urinating increases than normal bladder
- Overactive bladder – Urge to urinate even though the bladder is empty due to squeezing of bladder muscles randomly
- Discomfort – Sense of pressure in the lower abdominal region
- Dysuria – Condition of irritating or painful urination
- Nocturia – Required to urinate several times at or during night
- Enuresis – Bed wetting while sleeping
How can menopause urinary incontinence be treated or managed?
While urinary tract infection and urinary incontinence can be acutely managed using urine management device and catheters or women external catheter in healthcare settings, management strategies of UI are different for menopausal women.
Prescription medicine – Group of drugs known as antispasmodics can block the signals which cause the bladder muscles to spasm and urine to leak. These drugs are responsible for blocking muscarinic receptors located in the bladder.
Vaginal estrogen cream – A small dose of cream is applied inside the anatomy which can help to ease stress or urge incontinence.
Electric simulation – A sensor is inserted inside the anatomy and low electric current is stimulated to make pelvic floor muscles contract. This is done to have control over urination but it has been observed that various side effects are associated with it such as skin redness or allergy, discomfort, pain and itching.
Surgery – Sling procedure involves placing a small piece of mesh under the bladder neck to support the urethra, and colposuspension, to lift and reposition the bladder neck and urethra to improve support. Both procedures are typically performed through a small incision in the lower abdomen. However, surgery does come with risks such as infection and bleeding, and varying recovery time.
Urinary incontinence is an interdisciplinary problem combining medicinal, economic and social concerns. The data reveals that incontinence in postmenopausal women occurs more frequently than any other disease such as diabetes, hypertension or mental illness. It is observed that only one third of these women undergo treatment of incontinence. Unfortunately, people with this issue usually believe the only option for treatment is surgery and hence are afraid of performing it. But there are many effective and least invasive therapeutic methods to manage incontinence. Untreated incontinence could lead to many severe illnesses and degradation of quality of life.

2 replies on “Incontinence in Post-Menopausal Women”
Thinker Pedia very informative articles or reviews at this time.
NY weekly Great information shared.. really enjoyed reading this post thank you author for sharing this post .. appreciated